What Does It Mean To Have A Brca Mutation
According to Payal Shah, MD, a medical oncologist at Penn Medicine and assistant professor of medicine at the Hospital of the University of Pennsylvania, everyone has two copies of genes called BRCA1 and BRCA2, one copy inherited from each parent. BRCA1 and 2 are repair genes, so they help the body repair mistakes in DNA.
Karlena Lara-Otero, PhD, a genetic counselor at Stanford Health Care, says BRCA1 and 2 genes are specifically tumor suppressor genes that prevent cells from growing out of control, which is what leads to cancer. “When these genes work properly, they go to the site where cell damage occurs and repair it so cells can continue to function properly,” Lara-Otero tells Health.
The BRCA mutation can cause many types of cancer, but it’s most significantly associated with breast cancer. According to Lara-Otero, that’s because the BRCA gene is responsible for repairing DNA in breast tissue.
RELATED: What Is Metastatic Breast Cancer?
A BRCA mutation occurs when someone’s born with a copy of a BRCA gene that doesn’t suppress tumor growth effectively. This can lead to an increased risk of various cancers, such as breast and ovarian cancer, melanoma, pancreatic cancer, and prostate cancer.
Role Of Brca Mutations In The Modulation Of Response To Platinum Therapy
- 1Invictus Oncology Pvt. Ltd., Delhi, India
- 2Department of Biotechnology, Delhi Technological University, Delhi, India
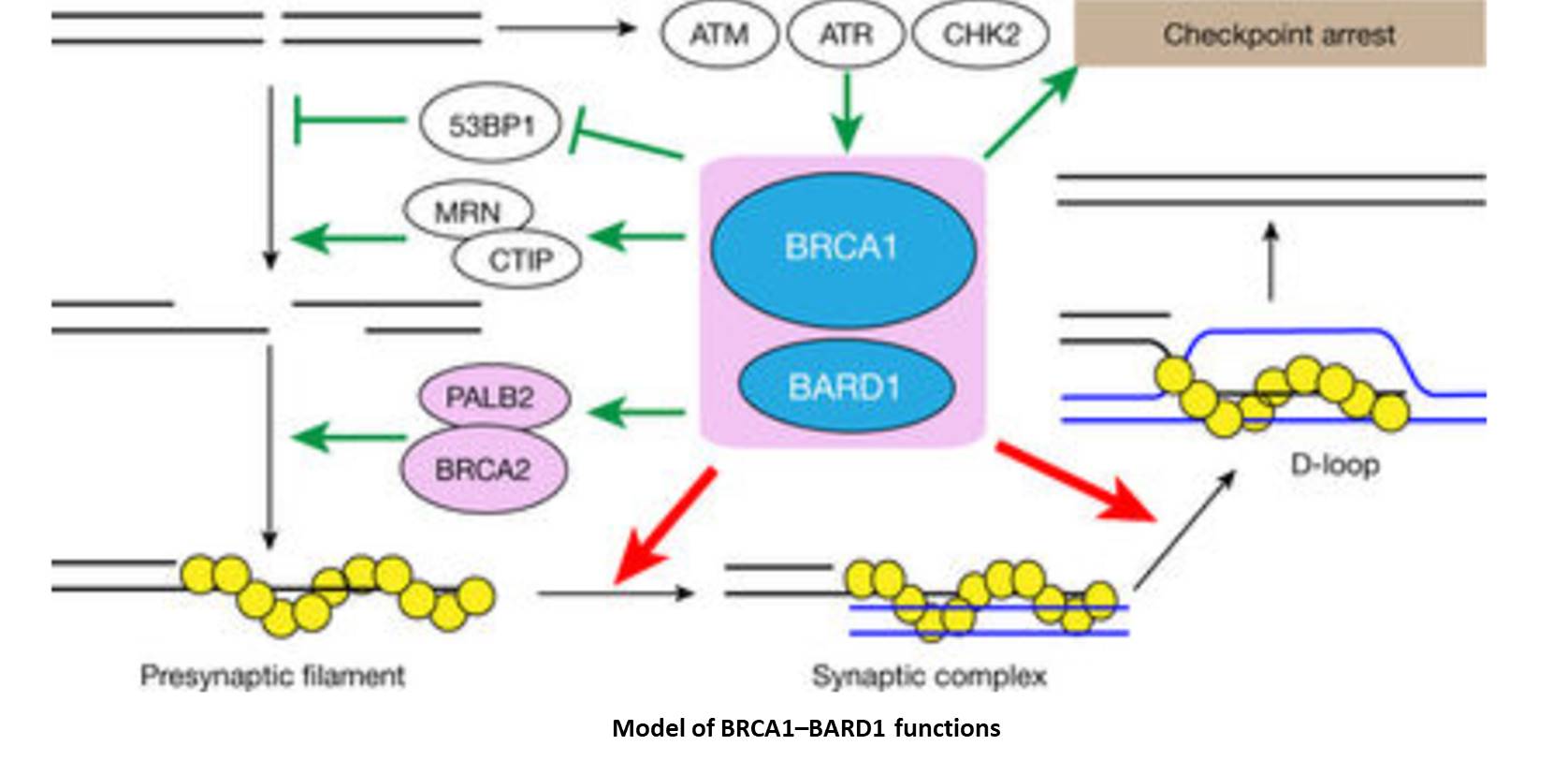
Recent years have seen cancer emerge as one of the leading cause of mortality worldwide with breast cancer being the second most common cause of death among women. Individuals harboring BRCA mutations are at a higher risk of developing breast and/or ovarian cancers. This risk is much greater in the presence of germline mutations. BRCA1 and BRCA2 play crucial role in the DNA damage response and repair pathway, a function that is critical in preserving the integrity of the genome. Mutations that interfere with normal cellular function of BRCA not only lead to onset and progression of cancer but also modulate therapy outcome of treatment with platinum drugs. In this review, we discuss the structural and functional impact of some of the prevalent BRCA mutations in breast and ovarian cancers and their role in platinum therapy response. Understanding the response of platinum drugs in the context of BRCA mutations may contribute toward developing better therapeutics that can improve survival and quality of life of patients.
The Brca1 And Brca2 Genes
The genes most commonly affected in hereditary breast and ovarian cancer are the breast cancer 1 and breast cancer 2 genes. About 3% of breast cancers and 10% of ovarian cancers result from inherited mutations in the BRCA1 and BRCA2 genes.
Normally, the BRCA1 and BRCA2 genes protect you from getting certain cancers. But some mutations in the BRCA1 and BRCA2 genes prevent them from working properly, so that if you inherit one of these mutations, you are more likely to get breast, ovarian, and other cancers. However, not everyone who inherits a BRCA1 or BRCA2 mutation will get breast or ovarian cancer.
Everyone has two copies of the BRCA1 and BRCA2 genes, one copy inherited from their mother and one from their father. Even if a person inherits a BRCA1 or BRCA2 mutation from one parent, they still have the normal copy of the BRCA1 or BRCA2 gene from the other parent. Cancer occurs when a second mutation happens that affects the normal copy of the gene, so that the person no longer has a BRCA1 or BRCA2 gene that works properly. Unlike the inherited BRCA1 or BRCA2 mutation, the second mutation would not be present throughout the persons body, but would only be present in the cancer tissue.
If you are concerned that you could have a BRCA1, BRCA2, or other mutation related to breast and ovarian cancer, the first step is to collect your family health history of breast and ovarian cancer and share this information with your doctor.
You May Like: Breast Cancer Type 3
Are There Symptoms Of Brca Gene Mutation
No, there are no specific symptoms of breast cancers caused by a BRCA1 or BRCA2 gene mutation, but your doctor may recommend a test and appropriate screenings if you have risk factors.
We would hope that all BRCA-related cancers would be identified on mammograms or MRI scans when they are small enough to be treated more easily, says Euhus.
This is one reason why it helps to know whether or not you carry a mutation, he explains. The value of genetic testing is that it enables you to be proactive and get regular screening, so that if cancer does occur, it can be diagnosed early.
High Risk Assessment and Genetic Testing at Johns Hopkins
The Johns Hopkins Kimmel Cancer Center offers genetic counseling and high risk assessments for patients with a personal or family history of breast and ovarian cancer.
What Is My Cancer Risk If I Test Positive For A Brca Mutation

It is high. Having a BRCA mutation means you have a likelihood of 45% to 85% for developing breast cancer in your lifetime, along with a 10% to 46% chance of ovarian cancer, Euhus says.
Thats considerably more than the probability of breast cancer among the general population, which is about 12%, or about one in eight. Ovarian cancer is rarer, affecting less than 1% of the general U.S. population.
Read Also: What Is The Prognosis For Stage 4 Breast Cancer
Weighing The Risks And Benefits Of Genetic Testing
A health care provider or genetic counselor can help you decide whether genetic testing is right for you and your family.
Testing for a BRCA1/2 gene mutation only requires a blood or saliva sample, but there are risks and benefits to consider before testing. There can be physical, emotional and financial impacts of knowing your genetic status.
Testing costs are usually covered by health insurance for people who fall into one of the categories above .
Learn more about genetic testing.
Your Race And Ethnicity
Overall, white women are slightly more likely to develop breast cancer than African American women, although the gap between them has been closing in recent years. In women under age 45, breast cancer is more common in African American women. African American women are also more likely to die from breast cancer at any age. Asian, Hispanic, and Native American women have a lower risk of developing and dying from breast cancer.
Risk in different groups also varies by type of breast cancer. For example, African American women are more likely to have the less common triple-negative breast cancer.
You May Like: Cure Stage 4 Breast Cancer
How It Is Done
The health professional taking a sample of your blood will:
- Wrap an elastic band around your upper arm to stop the flow of blood. This makes the veins below the band larger so it is easier to put a needle into the vein.
- Clean the needle site with alcohol.
- Put the needle into the vein. More than one needle stick may be needed.
- Attach a tube to the needle to fill it with blood.
- Remove the band from your arm when enough blood is collected.
- Put a gauze pad or cotton ball over the needle site as the needle is removed.
- Put pressure on the site and then put on a bandage.
Does Ethnicity Affect Risk For Harmful Brca1 And Brca2 Mutations
Anyone may inherit these gene mutations, but in the United States, they are found most commonly in those of Ashkenazi Jewish ancestry. The NCI says about 2 percent of Ashkenazi Jews carry the harmful variant in one of these two genes. Black women in the United States also tend to have BRCA1 variants unique to their racial group.
You May Like: Did Anne Hathaway Have Breast Cancer
Sporadic Cancer And Brcaness
BRCA1/2 mutations, seen most commonly in familial breast and ovarian tumors, impact the DNA repair pathway leading to genomic instability. However, some sporadic tumors that contain wild-type BRCA1 also have defective DNA repair pathway that may have resulted via other mechanisms. These characteristics of sporadic tumors that are similar to familial cancers are collectively called BRCAness. Inactivation of BRCA1 in sporadic breast and ovarian tumors may be brought about by non-genetic mechanisms like promoter methylation that result in lowering of gene expression to undetectable levels and loss of heterozygosity. In contrast, BRCA2 inactivation does not occur by promoter hypermethylationa significant number of sporadic breast and ovarian tumors show amplification of EMSY at the gene level. As discussed earlier, EMSYBRCA2 interaction may regulate DNA repair via HRR pathway . A common feature that both BRCA-mutated cancers and those showing characteristics of BRCAness share is the elevated susceptibility to DNA cross-linking agents like platinum drugs and this has been the rationale for including these as therapeutic agents .
What Are The Estimated Cancer Risks Associated With Hboc
Cancer risks for women with HBOC
-
Lifetime risk of breast cancer 45% to 75%
-
Lifetime risk of ovarian cancer
-
BRCA1 gene mutation 25% to 40%
-
BRCA2 gene mutation 10% to 20%
-
Developing a second breast cancer 20% to 40%
Cancer risks for men with HBOC
-
Lifetime risk of breast cancer
-
BRCA1 gene mutation 1% to 2%
-
BRCA2 gene mutation 6%
-
BRCA1 gene mutation some increased risk
-
BRCA2 gene mutation 20%
-
Men with a BRCA2 gene mutation have a significantly increased risk of developing more aggressive prostate cancer before age 65 and therefore screening should begin at age 40.
Recommended Reading: What Is The Prognosis For Stage 4 Breast Cancer
How Is Hboc Inherited
Normally, each person has 2 copies of each gene in their bodys cells: 1 copy is inherited from a persons mother and 1 copy is inherited from a persons father. HBOC follows an autosomal dominant inheritance pattern. This means that a mutation needs to happen in only 1 copy of the gene for the person to have an increased risk of getting that disease. This means that a parent with a gene mutation may pass along a copy of their normal gene or a copy of the gene with the mutation. Therefore, a child who has a parent with a mutation has a 50% chance of inheriting that mutation. A sibling or parent of a person who has a mutation also has a 50% chance of having inherited the same mutation. However, if the parents test negative for the mutation , the risk to the siblings significantly decreases but their risk may still be higher than an average risk.
Patients With Breast Cancer
Women who had taken part in these studies were contacted again in 1992 to obtain a bloodsample and again in 1993 to obtain specific permission to use the sample for genetic studies. Allpatients included in the study gave informed consent for these analyses, and the protocol wasapproved by the Ethical Committee of the Royal Marsden Hospital National Health ServiceTrust.
Don’t Miss: What Is Stage 3a Breast Cancer
A Rational Approach To Gene Mutations And Cancer Risk
Euhus stresses that not all genetic cancer risks are the same. Some genetic mutations increase the likelihood of cancer dramatically others, only by a few percentage points. These variations are important for doctors to understand, so they can work with the patient on a rational strategy for staying well.
Recommending any preventive treatment should be based on carefully calculating the actual risk to the patient. Practitioners can use tools to quantitatively calculate the probability of cancer, based on patient data. This extra attention can go a long way to avoid unnecessary, stressful and potentially harmful screenings, biopsies and surgeries.
Breast Cancer Treatment at Johns Hopkins
The breast cancer program at Johns Hopkins is made up of a diverse group of nationally-recognized specialists in breast cancer research and treatment.
Overcoming Platinum Resistance In Brca
Treatment failure as a consequence of development of resistance to platinum drugs resulting in disease recurrence is a major roadblock in clinical management of cancers that carry BRCA mutations. In such cases, non-platinum-based drugs can achieve improved response and extended survival. PARP-1 and PARP-2, members of the PARP family, recruit the base excision repair machinery, a parallel, but less efficient mechanism for repairing damaged DNA, to the site of single-strand DNA breaks. In the absence of PARP, these lesions persist resulting in stalling of the replication fork during DNA synthesis and formation of DSBs . The concept of synthetic lethality, the underlying premise of which is that functional depletion of two genes singly may not cause deleterious effect but together are lethal, was thus introduced to cancer therapeutics to develop better treatment strategies. This was mainly achieved by blocking the BER pathway by small molecule inhibitors against PARP in BRCA1/2-mutated cancers .
You May Like: What Percentage Of Breast Cancer Is Triple Negative
How Is Hboc Identified
Mutations in the BRCA1 or BRCA2 genes can be identified through a blood or saliva test. The usual method of testing, called standard gene sequencing, can find most BRCA mutations. There are other types of mutations called rearrangements, which include deletions or duplications in BRCA1 and BRCA2 that also may cause an increased risk for these cancers. Testing is also available for large rearrangements in BRCA1 and BRCA2.
After initial BRCA1 and BRCA2 genetic testing, additional testing may be recommended if:
- The results were negative, meaning no genetic mutation was detected
- A variant of uncertain significance was detected, which means that there is a genetic change, but it is not known how that change could affect cancer risk
Talk with your health care team and/or a genetic counselor for more information.
Most, but not all, insurance providers, including Medicare and Medicaid, cover the cost of complete BRCA1 and BRCA2 testing. Many genetic specialists offer multigene panels, which may include 6, 20, 40, or more genes depending on your personal and family history. The multigene panel tests may often be done at the same time as BRCA1 and BRCA2 testing. Talk with your genetic counselor for more information on the type of testing you will have and your insurance coverage before testing begins.
Who Should Get Tested For Brca Gene Mutations And How Does It Work
If you’re wondering whether you may have a BRCA mutation, the first step is to collect your family health history. If you have BRCA-related cancer in your family, you may be a candidate for testing. For example, Dr. Shah says a clinician may test people with relatives who had breast cancer at a young age. Currently, the U.S. Preventive Services Task Force recommends genetic testing to women with a personal or family history of breast, ovarian, fallopian tube, or peritoneal cancer or an ancestry associated with a BRCA1 or BRCA2 mutation.
As you collect your family health history, pay attention to certain details. “Make sure you have information on the types of cancers in your family, including the age of diagnosis, how the person is related to you, and whether they ever had any other genetic testing done for inherited cancers,” says Dr. Rana.
It’s also important to understand the limitations in your family history. For example, if your parent is an only child or your parent was adopted, Dr. Rana says that’s not the same as having no family history of cancer.
If you do have a family history of any cancers associated with BRCA mutations, bring it up to your doctor, who can help you determine whether you should undergo genetic testing. According to Dr. Rana, your doctor may also recommend genetic testing if you don’t know your family history and can’t access it.
You May Like: How To Cure Breast Cancer With Baking Soda
Recommendation Of Brca Pathogenic Variant Screening In Breast Cancer Patients
If a BRCA1/BRCA2 pathogenic variant is suspected, genetic testing is required. The American Society of Clinical Oncology and National Comprehensive Cancer Network recommend genetic testing if the BRCA pathogenic variant risk is high, with risk factors including family history of BRCA pathogenic variant, family history of breast or ovarian cancer, diagnosis of breast cancer or ovarian cancer, male breast cancer, onset of breast cancer at young age, and diagnosis of TNBC at age 60 years or younger . More detailed BRCA genetic testing criteria are as follows: there are more than three breast cancer patients in the family other than the patient, regardless of the age at diagnosis there are two breast cancer patients in the family and at least one was diagnosed at an age under 50 years the patient has breast cancer and another family member is diagnosed as having squamous ovarian cancer the patient has bilateral breast cancer the patient is diagnosed as having breast cancer at an age under 45 years and the patient is also diagnosed as having squamous ovarian cancer. The NCCN guidelines recommend BRCA genetic testing if a breast cancer patient has two or more family members with a history of pancreas cancer or has more than two third-degree relatives diagnosed as having prostate cancer .
What Difference Will This Project Make
Understanding how BRCA1 and BRCA2 mutations can lead to the development of breast cancer will allow us to help women who have a mutation to reduce their risk of developing breast cancer. This research will also provide us with knowledge for the creation of more tailored treatments for people with breast cancer in the future. Ultimately, this will ensure that people with breast cancer get the most effective treatments for them, giving everyone the best possible chance of survival.
You May Like: What Is Stage 3a Breast Cancer
Treatment Of Brca1/brca2 Pathogenic Variant Breast Cancer
Surgery and radiotherapy
The main treatment strategies for breast cancer are surgery and systemic treatment. One of the main concerns in surgical treatment of BRCA1/BRCA2 pathogenic variant breast cancer is whether the treatment outcome of breast-conserving surgery combined with radiotherapy is equivalent to that of radical mastectomy. There has been only one study thus far that compared the results according to the method of operation in BRCA1/BRCA2 pathogenic variant breast cancer . According to that study, no significant difference was observed between overall survival of two groups , while BCS group showed higher ipsilateral local recurrence rate than that of mastectomy group .
Radiation following BCS is omitted only in very exceptional cases. Given the role of BRCA in DNA repair, concerns about complications of radiation therapy in BRCA pathogenic variant breast cancer have been raised. However, a study by Pierce, et al. revealed no difference in radiation complication rates between BRCA pathogenic variant and sporadic breast cancers.
Chemotherapy
Poly polymerase inhibitor treatment